Therapeutic effect of natural killer T cell (CAR-NKT) therapy in immun…
페이지 정보
Author HK HIS Date19-09-16 18:19 View1,052 Comment0관련링크
본문
CAR-T is a therapeutic cure for cancer that has been on the market for the last two years. Many people do not know how to treat, but we know that CAR-T cell therapies are a long way off. Currently, only hematologic malignancies have been approved as treatments, and the adverse reactions to the immune response have been a major concern for researchers involved in this treatment. However, this research also shows new hope for patients with technology that minimizes side effects.
Latest Combined CAR-NKT Therapy
A new treatment for recurrent neuroblastoma patients is the CAR-NKT Cell Therapy (Clinical CMD-501, developed by Cell Medica, a UK cell company) in a joint clinical trial conducted by Bell Labor and Texas Children's Hospital in Houston. I was able to cure the cells.
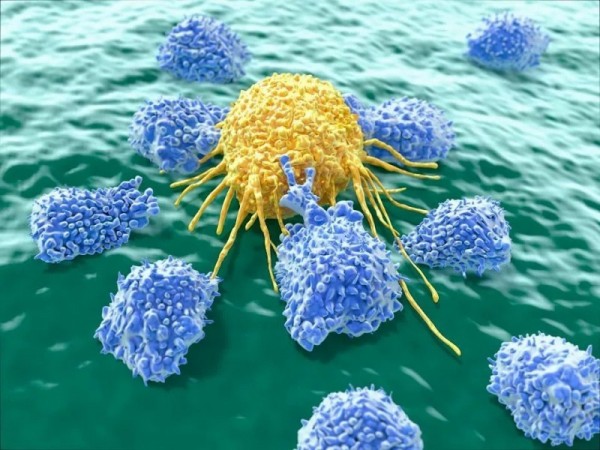
Immune and Adaptive Immunity
Natural killer T cell (NKT) cells are a kind of lymphoid cells. It is a lymphocyte that releases cytotoxic particles and destroys cancer cells. He is currently the first patient to receive genetically modified treatment of his NKT cells in two patients with neuroblastoma. This new treatment was used to treat recurrent neuroblastoma, a type of childhood cancer in which one in five is a cancer that is difficult to survive. Although most children can successfully treat most of the current treatment, the prognosis of children who have recurred after treatment with current treatment techniques is very poor and clinically inadequate. In the first clinical GINAKIT2 trial, we used CAR-NKT cells for the first time and treated two patients with metastatic cancer. Both patients will genetically modify their NKT cells and multiply molecules that target molecules called GD2. It is present in neuroblastoma and does not exist in normal cells. Cells are proliferated and injected into the patient again. Experimental Results: The first patient had improved disease for 4 weeks and the second patient had one of the two bone tumors completely disappeared and the other was slowly responding.
The FDA recently approved a second treatment for the patient. This is because the initial results were very good.
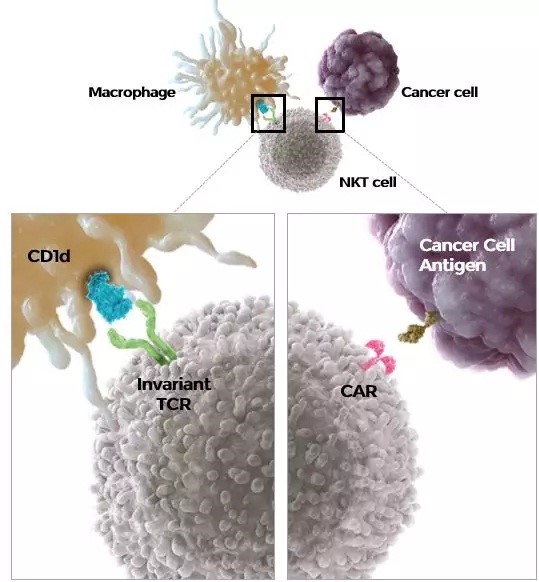
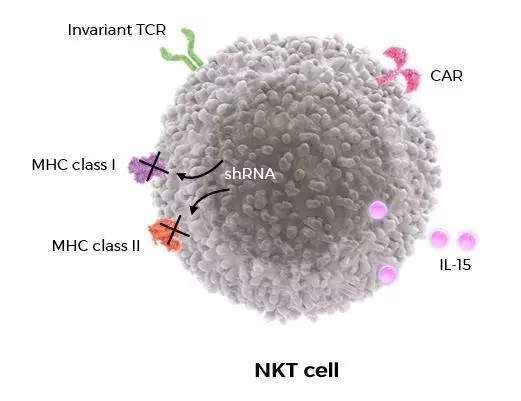
Although only two patients will not be able to draw much conclusions, at least two of these patients showed good initial signs after treatment. Stability is important at an early stage. In the early days of CAR-T cell therapy, life-threatening cell-factor-release syndrome (CRS) occurs, which can be controlled through additional treatments. These two patients did not experience these side effects. You should thoroughly evaluate the safety of your treatment and make sure that you take the appropriate measures to benefit more patients. The uniqueness of binding natural killer T cells (CAR-NKT), which can be applied to actual tumors, is that NKT cells or type 1 NKT cells are innate T lymphocytes, naturally present in tissues and include bone marrow. NKT (natural killer T) cells are special T cells with T cell receptor TCRs on the surface of one cell and NK cell receptors. NKT cells cause a lot of cell factor. In addition, the innovative CAR structure secretes IL-15 (leukocyte spot 15) to improve activity and persistence. Decreases in MCH levels 1 and 2 lead to improved endurance through the improvement of such cells.
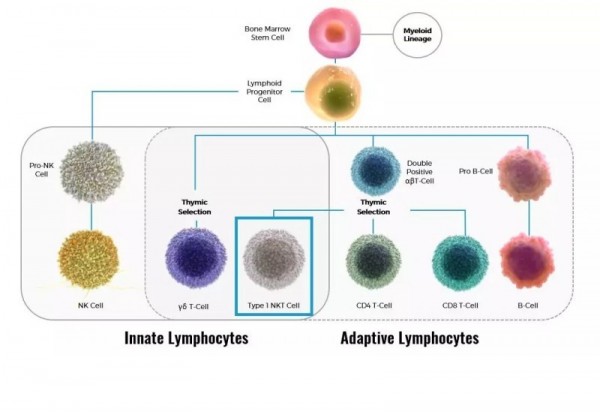
Enhanced persistence of CAR-NKT cells
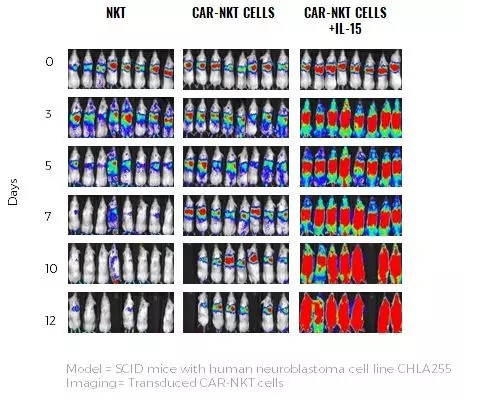
The graph above shows the results of animal experiments. CAR-NKT cells through the IL-15 modification process showed high increases and persistence.
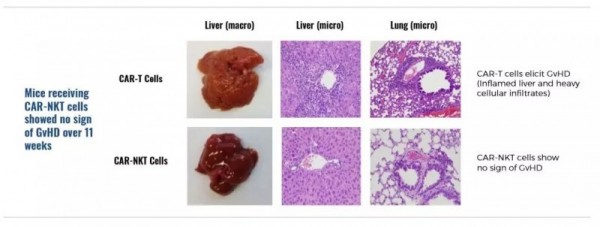
Pre-clinical data can confirm that NKT cells do not cause GvHD.
Advantages of Processed CAR-NKT Cell Therapy
Cancer is characterized by the rapid growth of normal cells. The first anticancer drugs are chemotherapy, which also attacks normal cells with omni-directional cell attack. These drugs were treatments to kill both fast-growing cancer cells and all cells together. Unfortunately, many normal cells in the body are also attacked, so there are many side effects, such as gastrointestinal toxicity, blood toxicity and even life threatening. As the molecular biology of cancer has evolved, we have come to discover specific cells and features of carcinoma. This finding has helped to develop targeted chemotherapy. Targeted chemotherapy has fewer side effects than older chemotherapy. Processed immune cells (NKT cells) are strategies that use a target to access specific cancer molecules. These methods have several advantages. Processed NKT cells have a specific target vector called the combined antigen receptor or CAR, which helps them find and kill cancer cells. Progressive NKT cells can prolong cell life and replicate through the patient's own cells and prevent long-term treatment and metastasis of newly developing cancer cells. Except for CAR, these NKT cells become natural tumor energy sources because these cells have unchanging T cell receptors. This power identifies some tumors, kills them directly and kills cells in the tumor, which in turn activates immunity to the tumor.
About neuroblastoma
Neuroblastoma is a cancer of the sympathetic nervous system that often occurs in children. It occurs in the neck, abdomen, and adrenal glands and can spread to bone marrow and other organs. Children with early neuroblastoma can be cured through surgery and chemotherapy, but half of them are at risk for recurrence, and surgery, radiation therapy, immunochemotherapy, and other treatments are needed.
About CMD-501
GD2 is a molecule expressed in almost all neuroblastomas and some other tumors. It is a good target for CAR-NKT cell therapy, which is not seen in normal tissues. CMD-501 is currently being developed to treat high-risk relapse-refractory neuroblastoma in children. CMD-501 is an autologous cell therapy for GD2. We are currently recruiting a first clinical trial in combination with NKT cell platform technology and genetic engineering CAR at Bell Medical School and Texas Pediatric Hospital. CAR-NKT cell studies are under way to treat various types of tumors.